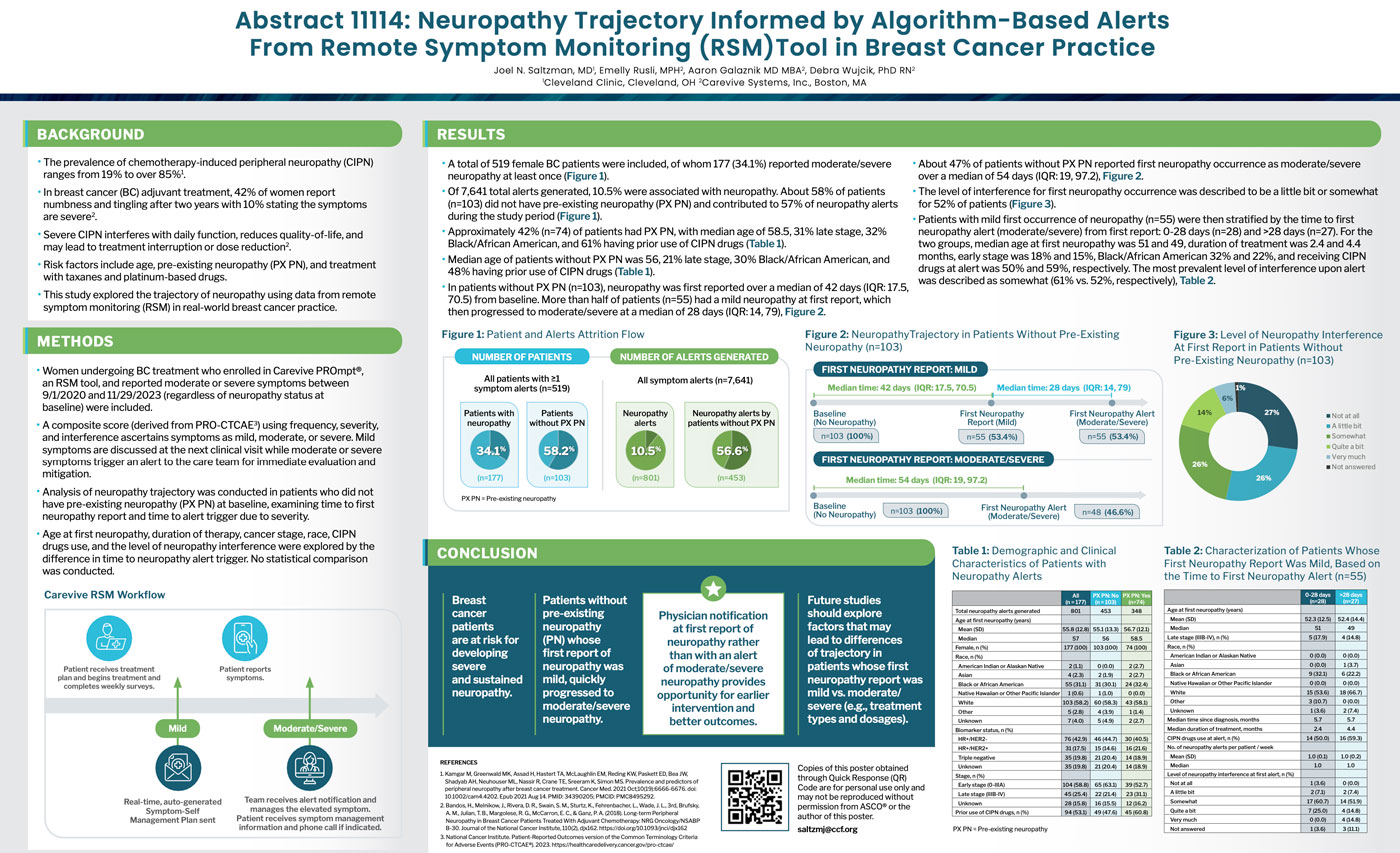
Authors: Joel N. Saltzman, MD1, Emelly Rusli, MPH2, Aaron Galaznik MD MBA2, Debra Wujcik, PhD RN2
1Cleveland Clinic, Cleveland, OH 2Carevive Systems, Inc., Boston, MA
Background
- The prevalence of chemotherapy-induced peripheral neuropathy (CIPN) ranges from 19% to over 85%1.
- In breast cancer (BC) adjuvant treatment, 42% of women report numbness and tingling after two years with 10% stating the symptoms are severe2.
- Severe CIPN interferes with daily function, reduces quality-of-life, and may lead to treatment interruption or dose reduction.
- Risk factors include age, pre-existing neuropathy (PX PN), and treatment with taxanes and platinum-based drugs.
- This study explored the trajectory of neuropathy using data from remote symptom monitoring (RSM) in real-world breast cancer practice.
Methods
- Women undergoing BC treatment who enrolled in Carevive PROmpt®, an RSM tool, and reported moderate or severe symptoms between 9/1/2020 and 11/29/2023 (regardless of neuropathy status at baseline) were included.
- A composite score (derived from PRO-CTCAE3) using frequency, severity, and interference ascertains symptoms as mild, moderate, or severe. Mild symptoms are discussed at the next clinical visit while moderate or severe symptoms trigger an alert to the care team for immediate evaluation and mitigation.
- Analysis of neuropathy trajectory was conducted in patients who did not have pre-existing neuropathy (PX PN) at baseline, examining time to first neuropathy report and time to alert trigger due to severity.
- Age at first neuropathy, duration of therapy, cancer stage, race, CIPN drugs use, and the level of neuropathy interference were explored by the difference in time to neuropathy alert trigger. No statistical comparison was conducted.
Results
- A total of 519 female BC patients were included, of whom 177 (34.1%) reported moderate/severe neuropathy at least once (Figure 1).
- Of 7,641 total alerts generated, 10.5% were associated with neuropathy. About 58% of patients (n=103) did not have pre-existing neuropathy (PX PN) and contributed to 57% of neuropathy alerts during the study period (Figure 1).
- Approximately 42% (n=74) of patients had PX PN, with median age of 58.5, 31% late stage, 32% Black/African American, and 61% having prior use of CIPN drugs (Table 1).
- Median age of patients without PX PN was 56, 21% late stage, 30% Black/African American, and 48% having prior use of CIPN drugs (Table 1).
- In patients without PX PN (n=103), neuropathy was first reported over a median of 42 days (IQR: 17.5, 70.5) from baseline. More than half of patients (n=55) had a mild neuropathy at first report, which then progressed to moderate/severe at a median of 28 days (IQR: 14, 79), Figure 2.
- About 47% of patients without PX PN reported first neuropathy occurrence as moderate/severe over a median of 54 days (IQR: 19, 97.2), Figure 2.
- The level of interference for first neuropathy occurrence was described to be a little bit or somewhat for 52% of patients (Figure 3).
- Patients with mild first occurrence of neuropathy (n=55) were then stratified by the time to first neuropathy alert (moderate/severe) from first report: 0-28 days (n=28) and >28 days (n=27). For the two groups, median age at first neuropathy was 51 and 49, duration of treatment was 2.4 and 4.4 months, early stage was 18% and 15%, Black/African American 32% and 22%, and receiving CIPN drugs at alert was 50% and 59%, respectively. The most prevalent level of interference upon alert was described as somewhat (61% vs. 52%, respectively), Table 2.