Research to improve patient
Explore our current and
completed research studies.
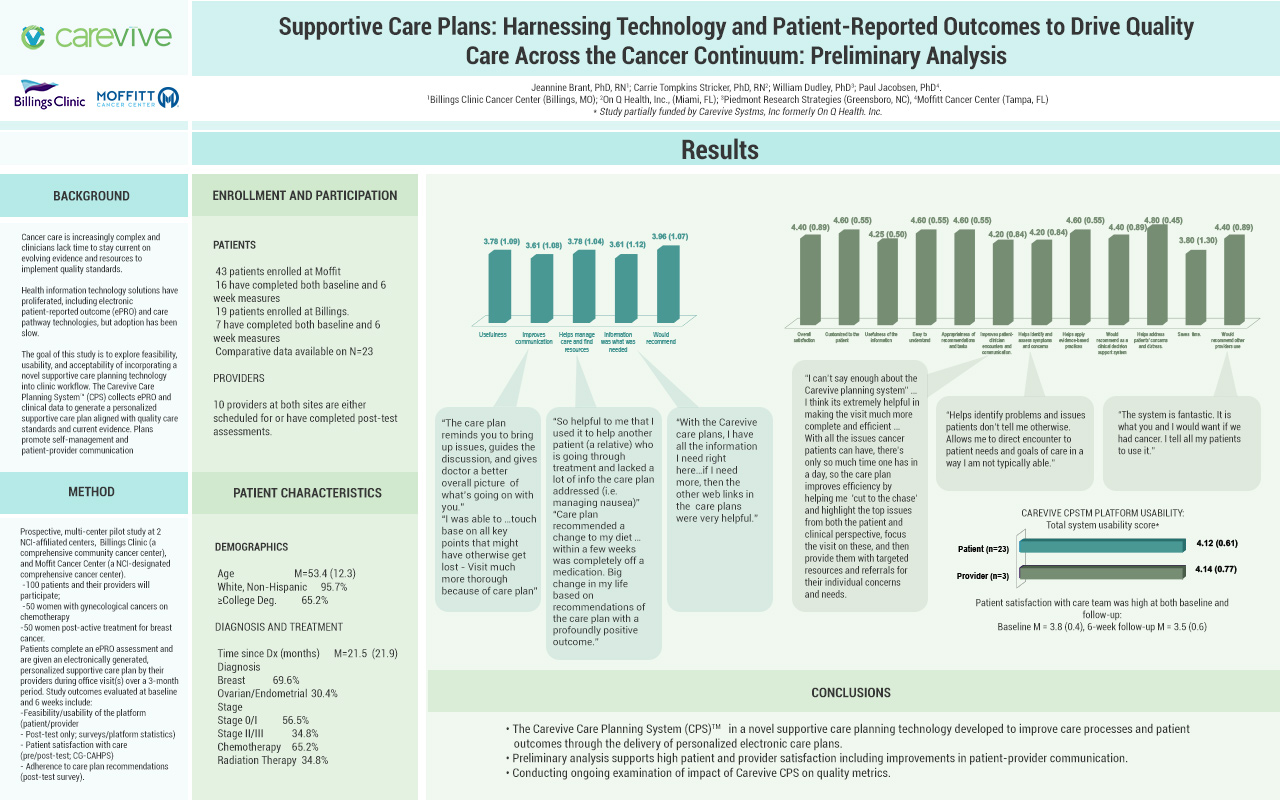
Driving quality of care across the cancer continuum by harnessing technology and patient-reported outcomes
Evidence-based supportive care should be integrated across the cancer continuum and include proactive symptom assessment and management strategies. The Carevive care planning system collects ePRO and clinical data to generate personalized, algorithm-driven supportive care plans (CP). In recent years, clinical studies have proven that the systematic collection of ePROs, along with nursing intervention, improves time on treatment and patient quality of life, while reducing ED visits and hospitalizations (Basch, 2017).
In this project, women with gynecological (GYN) cancers on chemotherapy or breast cancer post-active treatment completed ePRO assessments and were given electronically generated, personalized supportive CPs tailored to individual symptoms and local healthcare resources and designed to promote self-management and patient-provider communication.
Carevive improved care processes and patient satisfaction with the care team through the delivery of personalized electronic care plans aligned with quality care standards and current evidence.
Answers based on a one to five graded scale, where five is the highest rating.
Phase II is underway where clinical outcomes data of the treatment decisions are being collected. View poster.
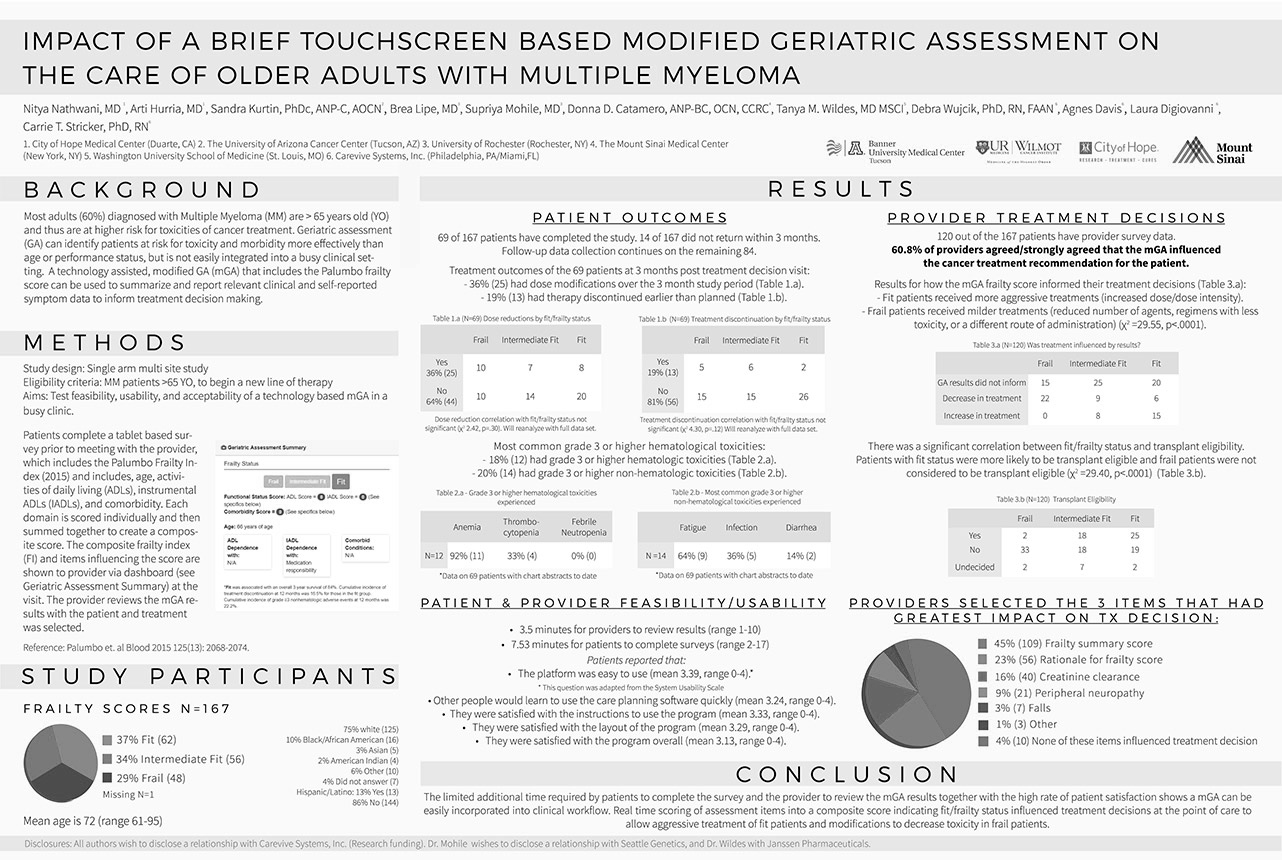
Improving treatment decision-making by implementing geriatric assessment
Age alone should not be used either to determine if a patient should receive treatment or to establish how much treatment is necessary. Using Carevive’s modified geriatric assessment (mGA), providers reviewed all relevant information to make a treatment recommendation that is tailored to the individual patient’s condition and needs. In the clinic setting, patients provided information about goals of care, needs and concerns along with functional assessment and other medical conditions on the Carevive tablet.
Results
In this study of older MM patients, 61.2 percent of treatment decisions were influenced by the mGA results by customizing the treatment regimen to accommodate the needs of the patient.
Cancer care delivery models that improve patient clinical and quality of life outcomes
Carevive is currently running a continuous improvement project in advanced NSCLC that joins the Carevive technology with clinical performance improvement processes, medical claims data analytics and financial performance to improve practice transformation. The program is implemented across three provider organizations participating in the Oncology Care Model (OCM). Aligned with the goal of OCM and the aims of the National Quality Strategy, the project’s objectives are to ultimately improve patient experience and care, lower costs and support better population health.
Study Objectives
Evaluate the a) Use of NSCLC molecular testing and treatment selection concordant with evidence-based guidelines, b) concordance between actual and patient-perceived goals of lung cancer therapy, c) documented patient values, concerns and preferences that align with treatment profiles (i.e., shared-decision making), d) health care utilization; specifically, ED visits and hospitalizations, e) appropriate timing and use of advanced care planning, f) integration of adjuvant palliative care services and g) reductions in overall costs of care for NSCLC patients.
Effectiveness of Shared Decision Making to advance care outcomes and provider-patient engagement
Shared decision-making (SDM) is a top priority for improving quality of healthcare delivery. SDM is an approach where clinicians and patients share the best available evidence when faced with the task of making decisions and where patients are supported to consider options to achieve informed preferences. In cancer, most patients desire an active or shared role in decision-making, yet 39 percent of patients experience discordance between preferred and actual decision-making roles, with most reporting less than desired involvement. Because there are numerous treatment options, aligning physician-patient goals of care and integrating patient preferences into a SDM model is particularly important for patients.
Study Objectives
In addition to feasibility and usability of the SDM model in practice to advance care, Carevive will also evaluate the correlation of the use of SDM to improve patient quality of care, treatment adherence and treatment sequencing.
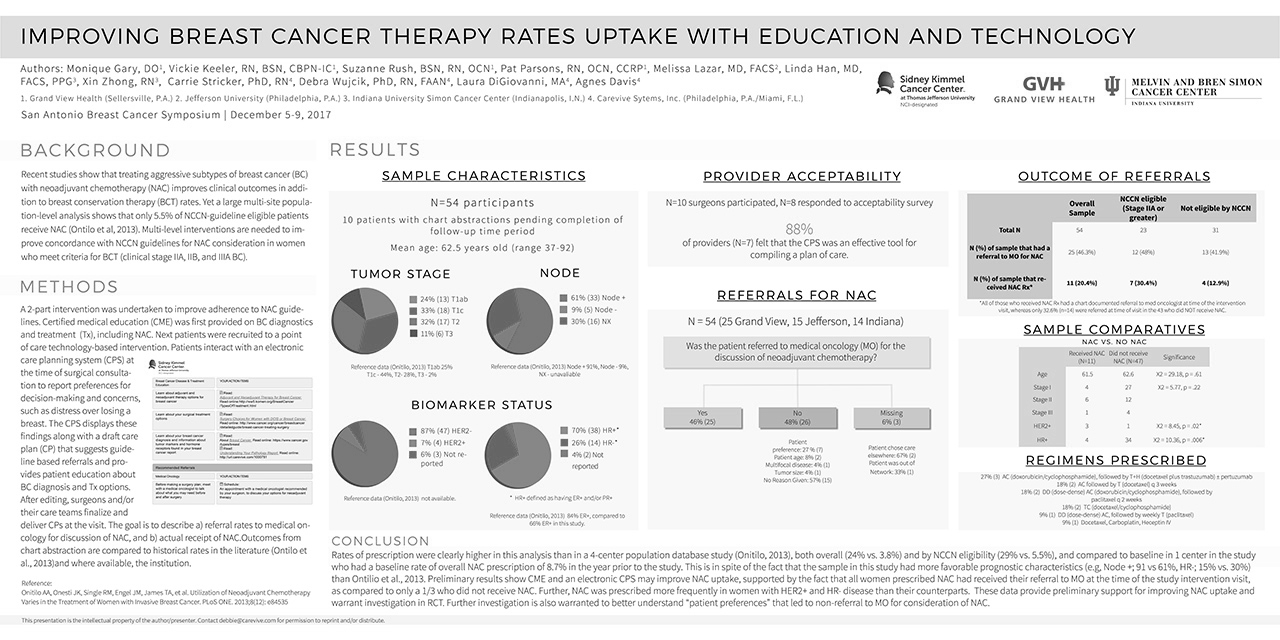
Improving breast cancer therapy options with education and technology
Recent studies show that treating aggressive subtypes of breast cancer with neoadjuvant treatment (chemotherapy plus breast-sparing surgery) improves clinical outcomes in addition to breast conservation therapy rates. Researchers leveraged Carevive technology in a two-part intervention study to capture patient concerns and preferences for decision-making, deliver patient care plans with guideline-based referrals and offer specific education on treatment options.
Results
Results demonstrate the application of education and use of Carevive’s care planning system increased referrals for breast-sparing treatment of breast cancer.