A cancer registry is a systematic collection of data about cancer and tumor diseases. The data are collected by Cancer Registrars. Cancer Registrars capture a complete summary of patient history, diagnosis, treatment, and status for every cancer patient in the United States, and other countries as well.
Lifetime follow-up is another important aspect of the cancer registry. Current patient follow-up serves as a reminder to physicians and patients to schedule regular clinical examinations and provides accurate survival information.
The Cancer Registry is continually growing in different ways and to be able to have the opportunity to show the data in a new and innovative way is stimulating and challenging.
For 2015, the Commission on Cancer’s Cancer Program Standards 2012, Version 1.2.1: Ensuring Patient – Centered Care (Standard 3.3) requires the development and implementation of a “process to disseminate a comprehensive care summary and follow up plan for patients who are completing cancer treatment.” With the survivorship plan being a hot topic right now, the registry has the capability to incorporate the data into the comprehensive care summary and follow up plan for the patient and the principal provider.
Carevive’s Care Planning System (CPS™) uses a sophisticated rules engine to generate personalized survivorship care plans at the point of care. Each care plan includes a treatment summary, follow-up and surveillance recommendations, possible late effects, hereditary cancer issues, ongoing symptoms, and health promotion recommendations. Our rules engine uses patient data – including family history, cancer diagnosis, systemic therapy, and optional patient-reported outcomes – to selectively apply evidence-based recommendations. For this process to work efficiently and effectively, these data must be structured, standardized, and timely.
When we built our Minimum Viable Product, released in 2014, we had no integration. All data was captured using a state-of-the-art survey engine, which stored patient data using proprietary code sets. This approach worked well for capturing patient-reported outcomes, but required clinicians to manually abstract the patient’s chart to capture family history, diagnosis, and treatment data, resulting in dual entry. See Exhibit A.
As we started investigating ways to eliminate this dual entry, through an automated feed from the cancer center’s EHR/EMR, we found that patient demographics and family history information is readily available using standard HL7 interfaces; however, cancer diagnosis and treatment information is currently stored in free-form progress notes and proprietary medical and radiation oncology management systems. That is, until it comes time to report these data to State Departments of Health.
When reporting cancer incidence data, health systems are required to report to central cancer registries using structured and standardized code sets – precisely the data needed for evidence-based survivorship care planning. A non-profit organization called the North American Association of Central Cancer Registries (NAACCR) has been in existence since 1987 to develop and drive adoption of “uniform data standards for the reporting of complete, accurate, and timely cancer incidence data.” After a deep dive with the cancer registry team at Virtua Health, Carevive engineers believed we could source most of the necessary data from Elekta’s METRIQ™ Cancer Registry. Hence, we created a proof of concept for breast cancer patients.
After three months of solution design, data mapping and testing, we are achieving 85% coverage of the data elements required for survivorship care planning and our proof of concept is now production ready. Virtua Fox Chase Cancer Program will start using our solution with breast cancer patients later this month.
Susan Van Loon, RN, CTR, Director of Oncology Data Services and Clinical Research at Virtua believes that the biggest pain point in developing a survivorship care plan is the treatment summary and that the key to having good registry data and integration is a proactive approach.
“The cancer registry is an ideal source for this information,” she stated, “since all of the required treatment summary information is collected, abstracted and coded following standardized rules in NAACCR format. Automating the treatment summary by using the registry data reduces valuable and limited time needed from the health care provider to manually complete this section of the survivorship care plan. Because Virtua participates in the Commission on Cancer’s Rapid Quality Reporting, we leverage that framework for the survivorship care plan. The Registry staff have now implemented a plan through a shared governance project to conduct concurrent abstracting of data for all primary sites to support both projects. Quality assurance processes have also been put in place by the cancer registry staff to ensure timeliness, completeness and accuracy of this data. The opportunity for the registry to participate in this project has enhanced the value and visibility of the cancer registry work at the cancer center administrative level. For cancer centers who want to use this approach my recommendation is to have a ‘registry champion’ within your organization who understands there is a plethora of untapped potential in using the registry data to create workflow efficiencies and you need a well-staffed registry department. Using three-to six-month old data should not be a barrier to initiate an Carevive integration effort. Once abstracted, it takes our registrars 5-10 minutes to pull data from our registry (the majority are breast and colon cancer patients)”.
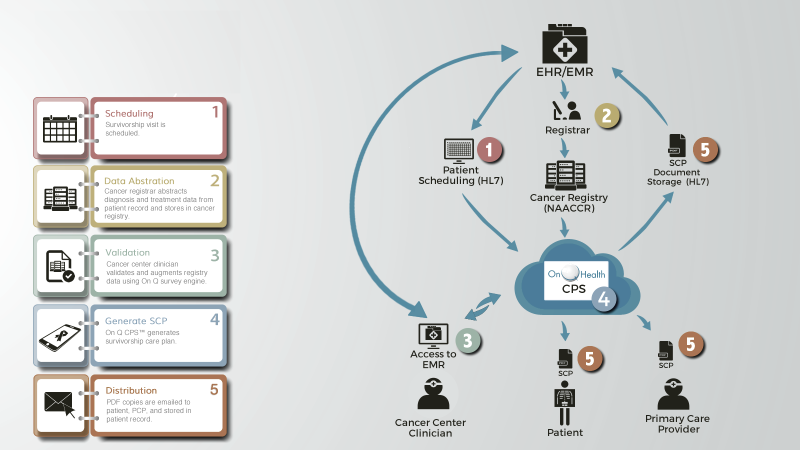
In the near-term Carevive is offering a hybrid solution that leverages HL7 interfaces for data we can source from the cancer center’s EHR/EMR and a NAACCR-compliant interface for data we can source from cancer registries to offer cancer center customers a relatively seamless integrated product that requires minimal to no manual entry of data to provide patients a survivorship care plan. See Exhibit B.
All of the EHR/EMR vendors we have spoken with have plans to provide access to structured and standardized oncology data leveraging the new HL7 Fast Healthcare Interoperability Resources (FHIR®) standard over the next 2 to 3 years. As such, Carevive can manage an affordable, phased, and seamless integration with cancer registry source systems, and EHR/EMR source systems with our cancer center customers. See Exhibit C.
In summary, the use of Carevive’s Care Planning System with HL7 and Cancer Registry integration is a great way to accelerate adoption of a content-rich solution for survivorship care planning, while positioning your survivorship program to leverage full HL7 integration as new interfaces become available.






