Authors: Omer Jamy, MD1, Stacey Ingram, MEd2, D’Ambra Dent2, William Dudley, PhD3, Matthew Dudley3, Julie Scott MSN4, Debra Wujcik, PhD4
- Division of Hematology and Oncology, UAB, Birmingham, AL;
- University of Alabama at Birmingham;
- Piedmont Research Strategies, Greensboro, NC;
- Carevive Systems Inc.
Background
- Acute Myeloid Leukemia (AML) is a disease of older patients
- NCCN guidelines recommend geriatric assessments as complementary for toxicity risk assessment in patients 60 years and older
- Utility of geriatric assessment (GA) in older AML patients in a real-world environment is not yet established
Objective
The primary objectives of this study were:
- to test the feasibility of using a modified GA (mGA), administered by patient self-report on a touchscreen computer, real-time use and utility by clinicians
- to determine the correlation of mGA results on treatment decision-making
Methods
Study Design
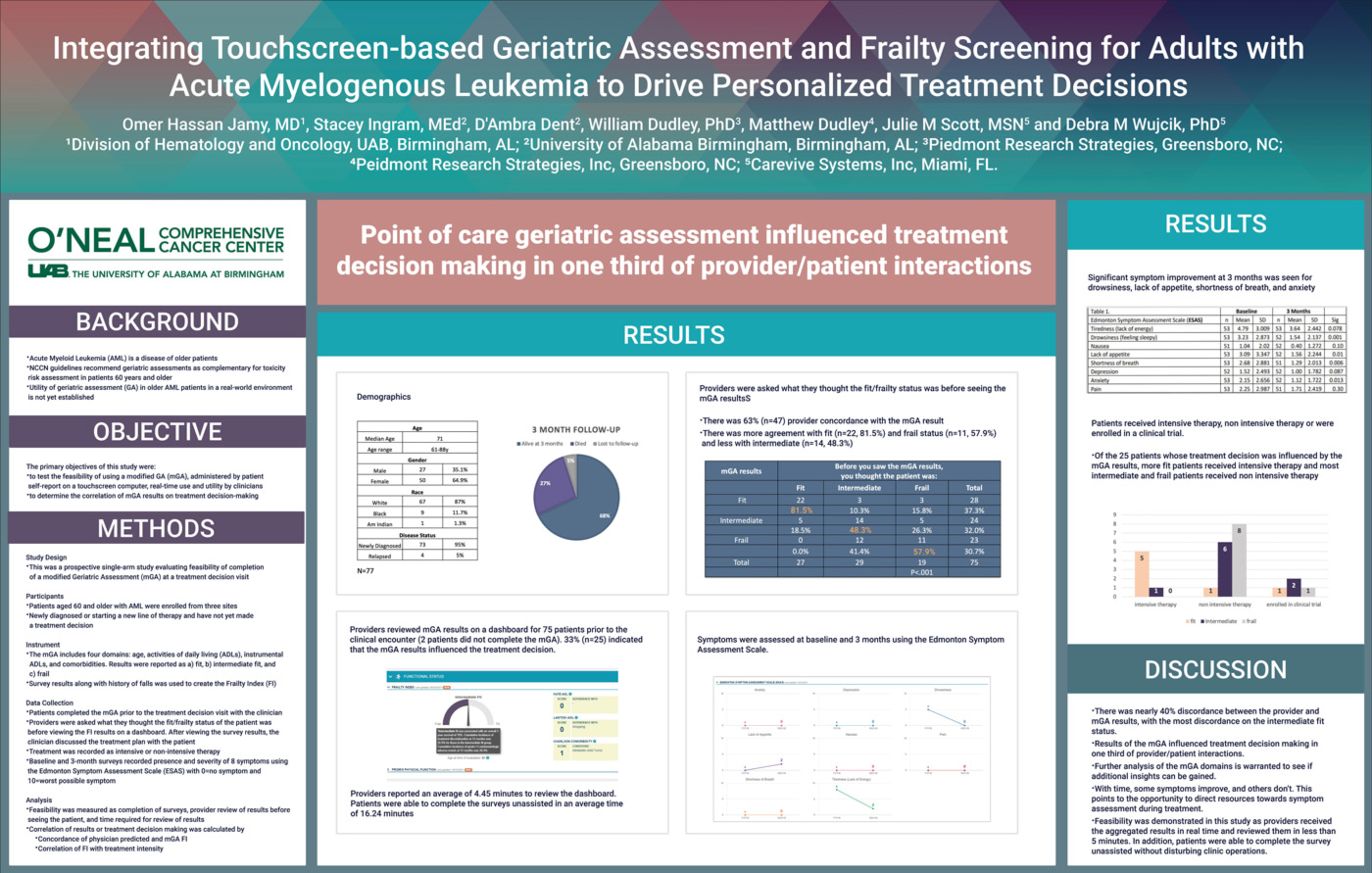
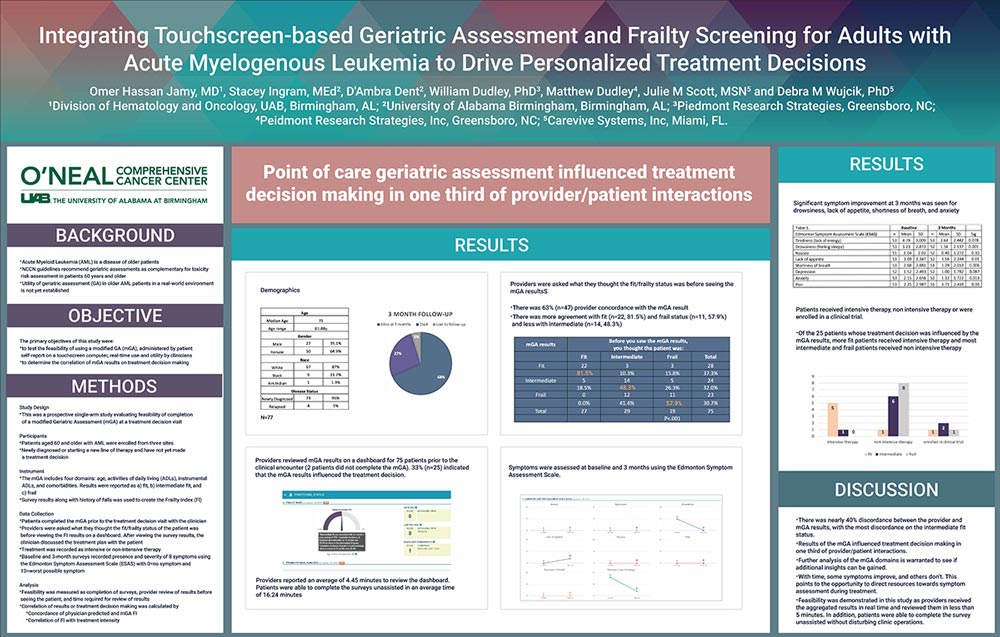
- This was a prospective single-arm study evaluating feasibility of completion of a modified Geriatric Assessment (mGA) at a treatment decision visit
Participants
- Patients aged 60 and older with AML were enrolled from three sites
- Newly diagnosed or starting a new line of therapy and have not yet made a treatment decision
Instrument
- The mGA includes four domains: age, activities of daily living (ADLs), instrumental ADLs, and comorbidities. Results were reported as a) fit, b) intermediate fit, and c) frail
- Survey results along with history of falls was used to create the Frailty Index (Fl)
Data Collection
- Patients completed the mGA prior to the treatment decision visit with the clinician
- Providers were asked what they thought the fit/frailty status of the patient was before viewing the Fl results on a dashboard. After viewing the survey results, the clinician discussed the treatment plan with the patient
- Treatment was recorded as intensive or non-intensive therapy
- Baseline and 3-month surveys recorded presence and severity of 8 symptoms using the Edmonton Symptom Assessment Scale (ESAS) with O=no symptom and 1 O=worst possible symptom
Analysis
- Feasibility was measured as completion of surveys, provider review of results before seeing the patient, and time required for review of results
- Correlation of results or treatment decision making was calculated by
- concordance of physician predicted and mGA Fl
- correlation of Fl with treatment intensity
Results
Significant symptom improvement at 3 months was seen for drowsiness, lack of appetite, shortness of breath, and anxiety.
Patients received intensive therapy, non intensive therapy or were enrolled in a clinical trial.
- Of the 25 patients whose treatment decision was influenced by the mGA results, more fit patients received intensive therapy and most intermediate and frail patients received non intensive therapy
Discussion
- There was nearly 40% discordance between the provider and mGA results, with the most discordance on the intermediate fit status.
- Results of the mGA influenced treatment decision making in one third of provider/patient interactions.
- Further analysis of the mGA domains is warranted to see if additional insights can be gained.
- With time, some symptoms improve, and others don’t. This points to the opportunity to direct resources towards symptom assessment during treatment.
- Feasibility was demonstrated in this study as providers received the aggregated results in real time and reviewed them in less than 5 minutes. In addition, patients were able to complete the survey unassisted without disturbing clinic operations.