Originally posted on Oncology Nursing News.
As nurses, we’re skilled at innovating. We have to be. The nature of our work means we often have to find new ways to help our patients. From new teaching methods to time-saving wound care techniques, every nurse has, at some point in his or her career, needed to think up something on the fly for the benefit of a patient.
This is innovation in action, and it’s at the heart of the MakerNurse movement. Started in 2013, MakerNurse focuses on identifying and fostering nursing innovation in hospitals across the United States.
Every day, nurses and technology specialists are working to improve cancer outcomes and make both the treatment and quality of life better for oncology patients. These innovators are using technology to develop products and services that guide cancer treatment, educate patients and families, and promote well-being and a positive outlook.
While these individuals come from different educational and professional backgrounds, they are blazing a trail in the treatment of cancer. They embody the spirit of the MakerNurse movement, using creativity to develop technological solutions in the fight against cancer.
Carevive Systems
It’s no secret that oncology care is complicated. Patients face a labyrinth of personal and financial challenges during their treatment. Treatment teams want to provide the best evidence-based care possible, but are challenged by the staggering amount of available information and troublesome reimbursement systems.
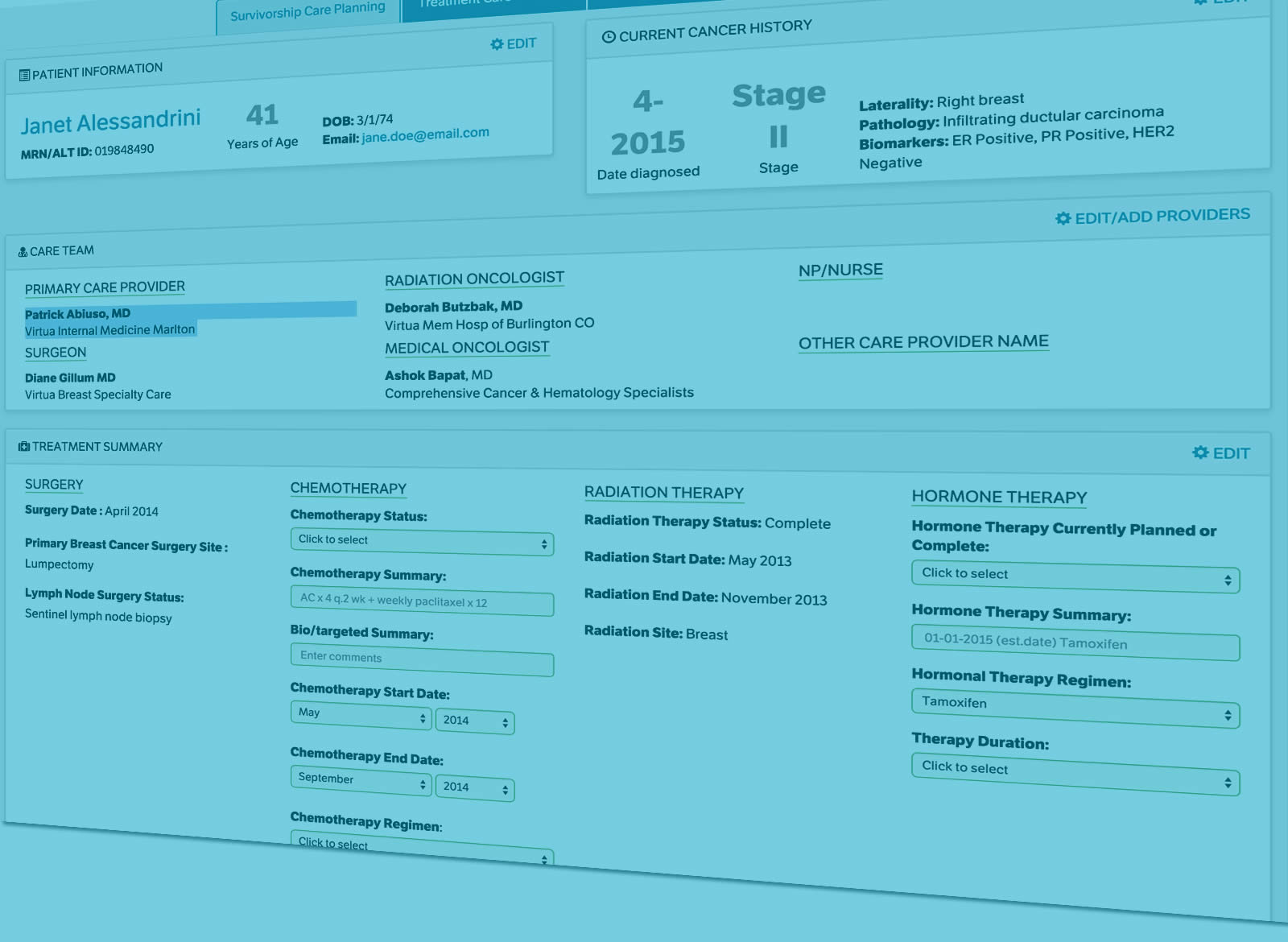
Carevive Systems, a company cofounded by Carrie Stricker, PhD, RN and Madelyn Herzfeld, BSN, RN, was formed in response to the need to provide more support for patients, families, and care teams.
The idea for Carevive started in 2007 after Stricker noticed a striking need for tools to help navigate the complex world of cancer care. With over 20 years of clinical practice and nursing research experience, Stricker had repeatedly witnessed her own patients’ difficulties in navigating through the healthcare landscape. She was inspired by the seminal Institute of Medicine 2005 report, Lost in Transition, to help address the reality that patients who weren’t receiving active treatment were “left behind” by the system.
In response, Stricker started to develop care plans to serve people transitioning from treatment to survivorship, but making these care plans was extremely time consuming and inefficient. Eventually, she realized that emerging technology offered the perfect opportunity to streamline the process. In collaboration with Herzfeld, Carevive was formed in 2013 (originally as On Q Health) to help develop care plans for all phases of the cancer experience, based on current research and patient priorities. It’s currently being used in 30 healthcare systems across the country.
Stricker explained that Carevive’s mission is to “provide clinical workflow tools and patient engagement solutions to help cancer centers in providing comprehensive, value-based care to individuals and families with cancer. The goal is to support patients, families, and survivors in navigating their cancer experiences with optimal quality of life, and as active members of the care team.”
To that end, Carevive’s cloud-based technology consumes and analyzes EMR and other clinical data sources, such as tumor registry data, along with patient-reported health data, to support the care team in planning patients’ treatment, managing their symptoms, and supporting their survivorship needs. The aggregated data gathered in this process also are used to provide insight into the real-world experiences of patients with cancer, enabling predictive analytics and to continuously improve outcomes.
Is Your Cancer Center Oncology Care Model Ready?
Learn how our survivorship care planning system can help with national standards and mandates. Carevive supports requirements for CMS Oncology Care Model (OCM) payment model and supports Commission on Cancer Accreditation Requirements for Distress Screening and Survivorship – providing a proactive, evidence-based symptom management care plan.
Request a Demo Today!
Based on the information reported, patients receive a personalized treatment plan for managing their personal symptoms. These patient-specific plans are focused on such areas as patient priorities, diagnostic data, evidence-based cancer treatment pathways, possible side effects, care and outcome goals, eligibility for clinical trials, and other resources.
Clinically, providers can use the reported information to prioritize concerns during patient visits, encouraging better communication and collaboration between the healthcare team and the patient. The healthcare team can also use reported patient information to map out trends in symptoms, side effects, and patient outcomes. With so much of oncology care funding and reimbursement driven by census, statistics regarding patient treatment at various facilities can help drive cancer costs in a more beneficial direction for all.





Nicely written article! I am always excited to see clinician-founded companies receive recognition!
Thank you Carol, she did great in capturing our value proposition and highlight our survivorship care planning platform!